Could my child have rosacea?
Few children and teens develop rosacea, but it’s worth considering if your child frequently has any of the following:
Red, irritated eyes
Styes or pinkeye (especially if your child received treatment)
Red, swollen eyelids that may itch and can look greasy or crusty
Long-lasting flushing on the face
Left untreated, rosacea can worsen. In children, the long-lasting flushing can progress to permanent redness in the middle of the face. Some children develop acne-like breakouts.
When rosacea affects the eyes, a child may continue to get styes and pinkeye. Even when you treat these, new styes and cases of pinkeye develop. This is often a warning sign of ocular (affects the eyes) rosacea, a condition that is often missed in children.
Red, swollen, and itchy eyelids can be another sign of ocular rosacea.
Without treatment for ocular rosacea, your child can continue to get styes and pinkeye. Eyelids can continue to turn red and swollen and then clear. Your child’s eyes may become extremely sensitive to light or feel gritty most of the time.
As the rosacea progresses, an open sore can develop on an eye. This is a serious medical problem because an open sore can lead to partial or complete loss of eyesight.
Treating the eyes can prevent ocular rosacea from progressing. Treatment can also get rid of the frequent styes, pinkeye, and other signs of ocular rosacea. When treated early, ocular rosacea responds well to treatment.
To find rosacea early, it helps to see a doctor who has expertise in diagnosing skin conditions, such as a board-certified dermatologist.
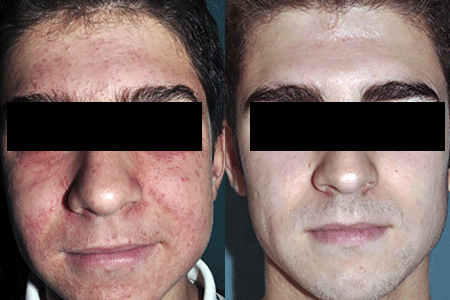
Before and after treatment for childhood rosacea
Rosacea covered much of this 13-year-old boy’s face (left), but 4 months after beginning treatment, his skin is clear (right).
How do dermatologists find rosacea in children?
Your dermatologist will carefully examine your child’s face and eyes, looking for signs of rosacea.
When a child has signs of rosacea on the skin, a board-certified dermatologist will want to rule out more common childhood diseases that can look like rosacea. This list includes acne, skin infections, and allergic skin reactions. To rule out other conditions, your child may need a medical test, such as a blood test.
How to prepare for this dermatology appointment
Your dermatologist will want to know whether your child has a high risk of developing rosacea. To find out, your dermatologist may ask the following questions:
Do any of your child’s close blood relatives have rosacea?
Does your child have any other medical conditions?
Has your child needed any medication, including medication that one takes and medication that you apply to the skin?
Being able to answer these questions can go a long way toward finding out whether your child has rosacea. On the day of the dermatology appointment, your child’s eyes, skin, or both may be clear. Rosacea can come and go.
If you don’t see redness or eye problems, your child can still have rosacea. Be sure to keep your dermatology appointment. Without treatment, rosacea can worsen.
How is rosacea treated in children and teens?
If your child or teen has rosacea, your dermatologist will tell you:
Where the rosacea appears (skin, eyes, both)
What treatment is recommended
When rosacea affects the skin, your dermatologist will talk with you about treatment. A typical treatment plan for a child or teen typically consists of lifestyle changes, medication to get the rosacea under control, and follow-up appointments.
If your child has mild ocular rosacea, your child’s dermatologist may treat that, too. For more severe ocular rosacea, your dermatologist can refer you to an eye doctor for treatment.
Here’s what a treatment plan for the skin often involves
Find and avoid what triggers your child’s rosacea. When a child has rosacea, many things can irritate the already sensitive skin and cause the rosacea to flare. What irritates (or triggers) one child’s rosacea may not trigger another child’s rosacea. That’s why you need to find out what triggers your child’s rosacea.
Apply sunscreen every day. To protect your child’s skin, dermatologists recommend applying sunscreen every day before your child goes outside. You want to apply the sunscreen to all skin that clothing won’t cover, such as the face, ears, and hands.
Avoid using makeup. Too often, these products contain ingredients that can irritate your child’s sensitive skin.
Before using any product that will touch your child’s skin, such as a skin or hair care product, read the list of ingredients. Any child who has rosacea should avoid products that contain sodium lauryl sulfate (often found in shampoo and toothpaste), menthol, or camphor.
Treat the rosacea as directed. Dermatologists prescribe both medication that you apply to the skin and medication that you take by mouth to treat a child with rosacea. When a child has mild or moderate rosacea, a medication called metronidazole is often applied to the skin. It’s typically applied once a day for 12 weeks to get the rosacea under control and then stopped.
Return for follow-up appointments. While this can be inconvenient, it’s important. Some children respond to one treatment but not another. Your child may need to continue using a medication for a bit longer than originally prescribed.
Getting rosacea under control can prevent it from progressing
The good news is that with treatment, rosacea can often be under control within a few weeks to months. Getting the disease under control helps to prevent it from progressing and allows your child to feel better.
Image
References
Miguel AI, Salagado MB, et al. “Pediatric ocular rosacea: 2 cases.” Eur J Ophthalmol.” 2012;22:664-6.
Noguera-Morel L, Gerlero P, et al. “Ivermectin therapy for papulopustular rosacea and periorificial dermatitis in children: A series of 15 cases.” J Am Acad Dermatol. 2017;76:567-570.
Orion C, Sfecci A, et al. “Idiopathic facial aseptic granuloma in a 13-year-old boy dramatically improved with oral doxycycline and topical metronidazole: Evidence for a link with childhood rosacea.” Case Rep Dermatol. 2016;8:197-201.
Prey S, Ezzedine K, et al. “IFAG and childhood rosacea: a possible link?” Pediatr Dermatol. 2013;30:429-32.
 Think sun protection during Skin Cancer Awareness Month
Think sun protection during Skin Cancer Awareness Month
 How to care for your skin if you have lupus
How to care for your skin if you have lupus
 Practice Safe Sun
Practice Safe Sun
 Sunscreen FAQs
Sunscreen FAQs
 Fade dark spots
Fade dark spots
 Hidradenitis suppurativa
Hidradenitis suppurativa
 Laser hair removal
Laser hair removal
 Scar treatment
Scar treatment
 Botox
Botox
 Kids' camp - Camp Discovery
Kids' camp - Camp Discovery
 Dermatologist-approved lesson plans, activities you can use
Dermatologist-approved lesson plans, activities you can use
 Find a Dermatologist
Find a Dermatologist
 Why choose a board-certified dermatologist?
Why choose a board-certified dermatologist?