Is there a best approach to widespread actinic keratoses?

By Deirdre Connolly, MD and Naomi Lawrence, MD
April 10, 2019
Vol. 1, No. 5
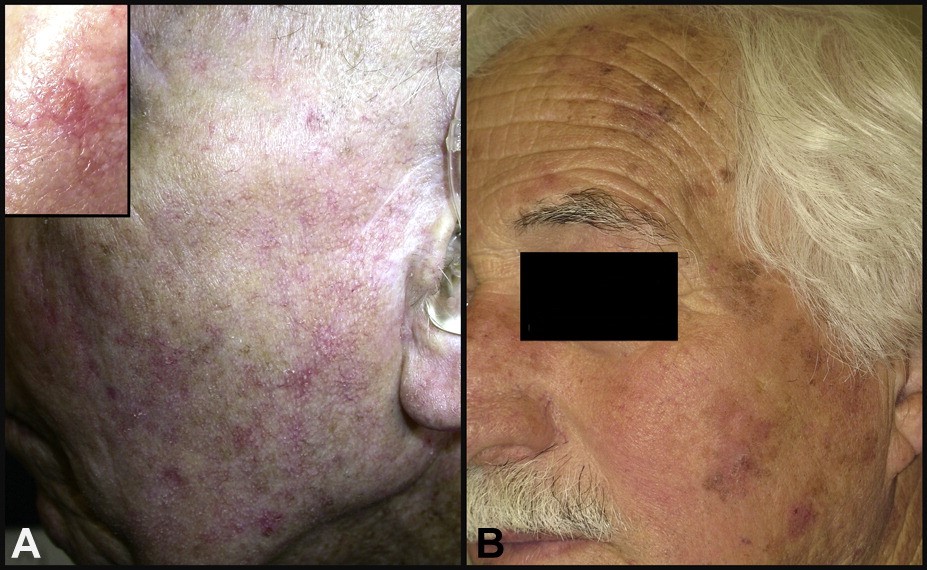
In a recent New England Journal of Medicine article, a large cohort was randomized to receive one of four treatments: 5-fluorouracil (5-FU), imiquimod, MAL-PDT, and ingenol mebutate. Of note, all AKs were curetted prior to treatment and the study was conducted in the Netherlands and utilized red light (or MAL-PDT), which is a more aggressive phototherapy regimen than is typically used in the United States (blue light, or ALA-PDT). The investigators followed up at 3 and 12 months, and considered failure less than 75% clearance of AKs. The study showed that 5-FU was associated with a significantly greater amount of treatment success than the other studied treatment modalities, with a 74.7% success rate, versus imiquimod (53.9%), MAL-PDT (37.7%), and ingenol mebutate (28.9%). The investigators noted that compliance was nearly 100% in the MAL-PDT and ingenol mebutate treatment groups and approximately 88% for the 5-FU and imiquimod treatment groups. In addition, patients expressed that they were unlikely to receive another MAL-PDT treatment due to the pain associated with the procedure. (2)
This study provides further evidence that 5-FU is the most effective field treatment for actinic keratoses. 5-FU is also a reasonably priced treatment option, with a course ranging from $80-135 with a GoodRx.com coupon. While 5-FU may clear actinic damage in a superior fashion than alternative treatment options, the question of whether it ultimately leads to fewer keratinocyte cancers, which is arguably the most important measure of its effectiveness, is not well established. In fact, a recent large comparative cohort study investigating the use of 5-FU and imiquimod for AKs concluded that 5-FU and imiquimod have similar short- or long-term effectiveness in the prevention of subsequent basal cell carcinoma, squamous cell carcinoma, and site-specific keratinocyte cancers. (3)
While efficacy in AK clearance is high with 5-FU, compliance remains the greatest obstacle because of its protracted treatment course and recovery. Medium depth peels offer a good compromise with nearly complete compliance and tolerable procedural discomfort. In addition, the skin is significantly improved within a week. (4,5) If the patient has a prior facial skin cancer, we submit for reimbursement and it is usually covered by Medicare. Chemical peels are a somewhat overlooked treatment option that in our experience clear actinic damage with equal efficacy to 5-FU but do not leave the patient hesitant to pursue further field treatment down the line. As we all well know, treatment of actinic damage must be thought of in terms of maintenance rather than cure, thus the ability to offer a field treatment that is well tolerated and efficacious will ultimately offer the best chance at preventing progression to skin cancer.
Point to remember: Of the most commonly used topical field therapies for AKs, it appears that 5 fluorouracil is the most effective. Patients must be advised to have long-term follow-up, and in all likelihood, will require repeated treatments and adjunctive therapies.
Our editor's viewpoint
Warren R. Heymann, MD
We all have patients burdened by multiple AKs who are a therapeutic challenge — patients know that I would love to dip them entirely in liquid nitrogen (I do not perform chemical peels — those patients get referred). Drs. Connolly and Lawrence discuss a truly important article comparing different options for patients with multiple AKs. By using a 75% clearance threshold as a measure of success, it is disappointing that all treatments could be considered failures, with 5-FU being the best among inadequate therapies. We need to be honest with our patients — topical therapies, of which 5-FU appears to be most efficacious, help reduce the AK burden, but will not be curative. Long-term follow-up is mandatory. Repeated courses of treatment, while being vigilant for the development of keratinocytic carcinomas, is essential. Regarding the choice of therapy, comparative studies such as Jansen et al, help narrow the field of field therapy. We need similar studies for all dermatologic conditions.
1) Lawrence N, Cox SE, Cockerell CJ, Freeman RG et al. A comparison of the efficacy and safety of Jessner's solution and 35% trichloroacetic acid vs 5% fluorouracil in the treatment of widespread facial actinic keratoses. Arch Dermatol. 1995 Feb;131(2):176-81.
2) Jansen MHE, Kessels JPHM, Nelemans PJ, Kouloubis N et al. Randomized Trial of Four Treatment Approaches for Actinic Keratosis. N Engl J Med. 2019 Mar 7;380(10):935-946.
3) Neugebauer R, Su KA, Zhu Z, Sokil M et al. Comparative effectiveness of treatment of actinic keratosis with topical fluorouracil and imiquimod in the prevention of keratinocyte carcinoma: A cohort study. J Am Acad Dermatol 2019; 80:998-1005
4) Kaminaka C, Yamamoto Y, Yonei N, Kishioka A et al. Phenol peels as a novel therapeutic approach for actinic keratosis and Bowen disease: prospective pilot trial with assessment of clinical, histologic, and immunohistochemical correlations. J Am Acad Dermatol. 2009 Apr;60(4):615-25.
5) Witheiler DD, Lawrence N, Cox SE, Cruz C et al. Long-term efficacy and safety of Jessner's solution and 35% trichloroacetic acid vs 5% fluorouracil in the treatment of widespread facial actinic keratoses. Dermatol Surg. 1997 Mar;23(3):191-6.
2) Jansen MHE, Kessels JPHM, Nelemans PJ, Kouloubis N et al. Randomized Trial of Four Treatment Approaches for Actinic Keratosis. N Engl J Med. 2019 Mar 7;380(10):935-946.
3) Neugebauer R, Su KA, Zhu Z, Sokil M et al. Comparative effectiveness of treatment of actinic keratosis with topical fluorouracil and imiquimod in the prevention of keratinocyte carcinoma: A cohort study. J Am Acad Dermatol 2019; 80:998-1005
4) Kaminaka C, Yamamoto Y, Yonei N, Kishioka A et al. Phenol peels as a novel therapeutic approach for actinic keratosis and Bowen disease: prospective pilot trial with assessment of clinical, histologic, and immunohistochemical correlations. J Am Acad Dermatol. 2009 Apr;60(4):615-25.
5) Witheiler DD, Lawrence N, Cox SE, Cruz C et al. Long-term efficacy and safety of Jessner's solution and 35% trichloroacetic acid vs 5% fluorouracil in the treatment of widespread facial actinic keratoses. Dermatol Surg. 1997 Mar;23(3):191-6.
All content found on Dermatology World Insights and Inquiries, including: text, images, video, audio, or other formats, were created for informational purposes only. The content represents the opinions of the authors and should not be interpreted as the official AAD position on any topic addressed. It is not intended to be a substitute for professional medical advice, diagnosis, or treatment.
DW Insights and Inquiries archive
Explore hundreds of Dermatology World Insights and Inquiries articles by clinical area, specific condition, or medical journal source.
All content solely developed by the American Academy of Dermatology
The American Academy of Dermatology gratefully acknowledges the support from Incyte Dermatology.
 Make it easy for patients to find you.
Make it easy for patients to find you.
 Meet the new AAD
Meet the new AAD
 2022 AAD VMX
2022 AAD VMX
 AAD Learning Center
AAD Learning Center
 Need coding help?
Need coding help?
 Reduce burdens
Reduce burdens
 Clinical guidelines
Clinical guidelines
 Why use AAD measures?
Why use AAD measures?
 Latest news
Latest news
 New insights
New insights
 Combat burnout
Combat burnout
 Joining or selling a practice?
Joining or selling a practice?
 Advocacy priorities
Advocacy priorities
 Promote the specialty
Promote the specialty