Race for the Case answers
Winter 2021 case by Rahul Nanda, MD, and Zeinah AlHalees, MD
An otherwise healthy 25-year-old male presented to the dermatology clinic with a two-week history of purpuric skin lesions following symptoms of sore throat, rhinorrhea, and malaise. He was not taking any medications and was not known for any allergies. His review of systems was notable for abdominal pain and arthralgias of the ankles and knees. On physical exam, palpable purpura extending from the feet to the mid-thighs were noted bilaterally. Additional workup revealed microscopic hematuria and mild proteinuria. The remainder of his workup was normal. A biopsy of a purpuric papule showed findings characteristic of the diagnosis on H&E, and direct immunofluorescence demonstrated perivascular IgA and C3 positivity.

What is the diagnosis and how should the biopsy ideally be performed? Answer: The diagnosis is that of an IgA vasculitis, a form of cutaneous small vessel vasculitis, also known as Henoch-Schönlein purpura in children.
A lesional biopsy for H&E should be done on an early purpuric papule of 48-72 hours duration, ideally without secondary changes.
Sampling for DIF is done similarly but is best performed on newly developed lesions of <24 hours duration.What are the characteristic findings seen on H&E? Answer: Findings are that of a leukocytoclastic vasculitis, which includes a transmural infiltration of the walls of small vessels (mainly in the superficial-mid dermis) by neutrophils undergoing nuclear karyorrhexis, and fibronoid necrosis of the vessel walls with red blood cell extravasation. Leukocytoclasia or “nuclear dust,” which is degranulation and fragmentation of neutrophils may also be seen.
Of note, biopsies of late lesions may not show these classic findings.What are the extracutaneous manifestations that may be seen in association with this diagnosis? Answer: Extracutaneous manifestations include arthralgias/arthritis in 75% of cases, most commonly involving the knees and ankles, GI involvement in 50-75% of cases, including colicky pain, GI bleed, and less commonly intussusception, and renal involvement with proteinuria/hematuria in 40-50% of cases. Adults are much more likely to develop chronic renal insufficiency, especially if they have an associated fever and increased ESR. Rarely, orchitis and lung involvement can occur.
What are a few conditions that are associated with this diagnosis? Answer: The most common association with IgA vasculitis is upper respiratory tract infection and vasculitis typically presenting 1-2 weeks following infection, especially in children. Although studies have reported positive antistreptolysin O titers in patients with IgA vasculitis, no causal relationship has been demonstrated. In adults, IgA vasculitis can occasionally be associated with malignancy. Unlike in cutaneous small vessel vasculitis, where malignancy is usually hematologic, patients with IgA vasculitis are more likely to have a solid organ malignancy (lung cancer most common).
How would you manage a patient with this diagnosis? Answer: IgA vasculitis is often self-limited and usually requires supportive management only, with spontaneous resolution in weeks-months. General measures include avoidance of tight clothing and leg elevation. Dapsone and colchicine can decrease the duration of skin lesions and frequency of recurrences. Prednisone and other immunosuppressives can be used to treat arthritis and abdominal pain associated with IgA vasculitis, but do not seem to prevent chronic renal failure in these patients. Lastly, long-term follow up of renal function with serial urinalysis and creatinine level is required.
References
Bolognia J, Schaffer JV, Cerroni L. Dermatology. 4th ed: Philadelphia, Pa.: Elsevier; 2018 9th November 2017. 2880
Winter 2021 winner
Congrats go out to Katelin Harrell, MD, a PGY-3 dermatology resident at University of Oklahoma Health Sciences Center. She correctly identified IgA vasculitis and gave the most comprehensive answers in the quickest time. If you win the latest case, there may be a Starbucks gift card in your future and your name in the next Directions!
Related Academy resources
Download every Boards Fodder in PDF format.
Keep up with current dermatologic literature and how to use the information in practice.
Access the archive of Directions in Residency.
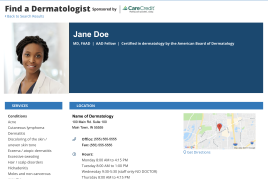 Make it easy for patients to find you.
Make it easy for patients to find you.
 Meet the new AAD
Meet the new AAD
 2022 AAD VMX
2022 AAD VMX
 AAD Learning Center
AAD Learning Center
 Need coding help?
Need coding help?
 Reduce burdens
Reduce burdens
 Clinical guidelines
Clinical guidelines
 Why use AAD measures?
Why use AAD measures?
 Latest news
Latest news
 New insights
New insights
 Combat burnout
Combat burnout
 Joining or selling a practice?
Joining or selling a practice?
 Advocacy priorities
Advocacy priorities
 Promote the specialty
Promote the specialty
