Teledermatology toolkit
Teledermatology during the COVID-19 pandemic
Medicare guidance
The Centers for Medicare & Medicaid Services (CMS) released guidance on March 30, 2020 further broadening access to Medicare telehealth services so that beneficiaries can receive a wider range of services from their doctors without having to travel to a healthcare facility. CMS has issued an 1135 waiver which will allow Medicare to pay for office, hospital, and other visits furnished via telehealth across the country and including in patients’ places of residence starting March 1, 2020.
Here are key takeaways for your practice:
The Office for Civil Rights (OCR) will use discretion in collecting penalties for the “good faith use of telehealth.” To be clear, under this Notice, physicians may use popular applications that allow for video chats, including Apple FaceTime, Facebook Messenger video chat, Google Hangouts video, or Skype to provide telehealth without risk that OCR might seek to impose a penalty for noncompliance with the HIPAA rules. Physicians should not use Facebook Live, Twitch, TikTok, or other public-facing communication services. Physicians are encouraged, but not required, to notify patients of the potential security risks of using these services and to seek additional privacy protections by entering into HIPAA business associate agreements (BAA). Please review the Academy's resources on choosing the right vendor for your practice.
Dermatologists can bill for telehealth visits for any patient in any location as those restrictions have been lifted.
Dermatologists and non-physician clinicians can now provide virtual check-in services to both new and established patients.
CMS is allowing physicians and non-physician clinicians to provide virtual encounters for beneficiaries who have audio phones only.
CMS has also announced that the telephone codes are now acceptable to report for telehealth services provided to Medicare beneficiaries .
Virtual E/M visits are considered the same as in-person visits and are paid at the same rate as regular, in-person visits. You must utilize modifier 95 and a place of service (POS) code of 11 to receive reimbursement at the non-facility rate for Medicare. Virtual visits can also be based on medical decision making or time rather than documentation of history and/or physical exam in the medical record.
CMS is allowing that annual consent be obtained at the time the virtual service is rendered. Consent may be verbal or written and must be documented in the patient’s record.
Physicians and non-physician clinicians can provide telehealth services from their home while continuing to bill from their currently identified practice location without having to update this in their Medicare enrollment.
Medicare co-payments can be waived for Original Medicare Beneficiaries.
Dermatologists should code for these services with telehealth codes explained in further detail here.
Dermatologists can provide supervision to non-physician clinicians virtually through real-time audio/video technology.
For additional guidance, please see CMS FAQs (PDF).
Private payer coverage of telehealth
The AADA has proactively contacted more than 65 insurers to map coverage of telehealth services through telephone and video consults. The Academy has gathered a list of policy updates from private payers (Excel). Members have reported that insurers have provided inconsistent guidance on how to code these telemedicine encounters and which codes are covered. The AADA is requesting members report information by insurer to privatepayer@aad.org.
For questions, please email practicecenter@aad.org.
Managing your practice during the COVID-19 outbreak
With COVID-19 (coronavirus) cases reported across the U.S., dermatologists and their practices should engage in precautions to protect their patients, themselves, and their staff members and to help prevent further spread of the virus.
Learn more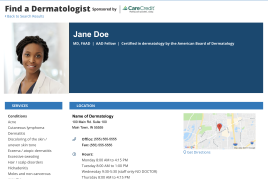 Make it easy for patients to find you.
Make it easy for patients to find you.
 Meet the new AAD
Meet the new AAD
 2022 AAD VMX
2022 AAD VMX
 AAD Learning Center
AAD Learning Center
 Need coding help?
Need coding help?
 Reduce burdens
Reduce burdens
 Clinical guidelines
Clinical guidelines
 Why use AAD measures?
Why use AAD measures?
 Latest news
Latest news
 New insights
New insights
 Combat burnout
Combat burnout
 Joining or selling a practice?
Joining or selling a practice?
 Advocacy priorities
Advocacy priorities
 Promote the specialty
Promote the specialty
